BEYOND THE MUMPS:LESSONS FROM INDONESIA’S RECENT OUTBREAK
By: Erni, Adhella Menur
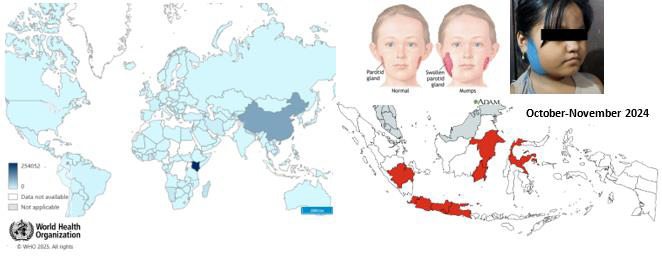
The mumps outbreak in Indonesia
The earliest description of mumps as a disease dates back to the 5th century BC by Hippocrates. One notable passage describes: “Swellings appeared about the ears, in many on either side, and in the greatest number on both sides. They were of a lax, large, diffused character, without inflammation or pain, and they went away without any critical sign.†Although mumps is generally a self-limiting disease, it is associated with rare but potentially serious complications, including deafness, orchitis, oophoritis, pancreatitis, and meningitis. The virus that caused the disease was first identified in 1934, and the first mumps vaccine, known as Mumpsvax, was developed in 1967 by Maurice Hilleman. The vaccine was created using a strain of the mumps virus that had infected his five-year-old daughter, Jeryl Lynn Hilleman. The combination vaccine containing live attenuated viruses for measles, mumps, and rubella (MMR) was introduced around 1971. Currently, 123 of the 194 (63.4%) WHO member countries have included the MMR vaccine in their national immunization programs. While the discovery of the mumps vaccine has significantly reduced the number of cases globally, mumps remains less well-controlled compared to measles and rubella. Between 1999 and 2019, approximately 500,000 mumps cases were reported annually to the WHO. Several mumps outbreaks occurred in many countries. Even in highly vaccinated populations, such as in the United States, outbreaks still occur. For example, a 2006 outbreak involved over 6,500 cases in the US, mostly among vaccinated university students aged 18–24, with 84% having received two doses. Similarly, a 2009–2010 outbreak saw over 3,500 cases in vaccinated adolescents aged 13–17, with 89% receiving two doses.
The rate of mumps incidence in Indonesia is challenging to estimate because mumps is not a notifiable disease and is not included in annual reports to the national or WHO database. The actual number of mumps cases in Indonesia is likely much higher, as mumps vaccination is not part of the routine immunization program. The MMR vaccine is available only in private healthcare facilities, costing approximately $42 USD (700,000 Rupiahs). The surge in mumps infections in Indonesia has been notably high, particularly in the past few months. In late 2024, several schools reported a significant increase in mumps cases, known as gondongan in Indonesian language, spreading rapidly among students. On October 30, 2024, the Directorate General of Disease Prevention and Control released a circular letter urging heightened precautions for mumps, emphasizing case reporting through event-based surveillance and proper case management.
By November 2024, suspect mumps cases nationwide had reached 6,593. The provinces with the highest reported cases included East Java, Central Java, West Java, Banten, Jakarta, Yogyakarta, East Borneo, South Sumatra, South Sulawesi, South Borneo, and Central Sulawesi. Specific regional data showed an estimated 2,001 cases in Malang, 1,596 cases in Jombang, 907 cases in Banyuwangi, 621 cases in Rembang, and 215 cases in Kediri. The Jakarta Health Office alone reported nearly 30,000 cumulative mumps cases from January to November 2024.
The mumps outbreak in Indonesia highlights significant gaps in immunization coverage and the challenges of high population density. Additionally, mumps has been largely neglected compared to other infectious diseases, as it often presents with mild symptoms. This underestimation allows the highly contagious disease to spread unchecked. Mumps can still lead to serious complications, potentially imposing a substantial burden on individuals and the healthcare system. Further-more, the misuse of antibiotics to treat this viral infection raises an even more critical concern about the growing threat of antimicrobial resistance. In this edition, we will delve into this of-ten-overlooked yet preventable viral infection.
The virus behind the outbreak
The mumps virus (MuV) is a non-segmented neg-ative-strand RNA virus from a member of the Paramyxoviridae family. The structure of the virus consists of an enveloped core decorated by spike form glycoprotein called mumps hemagglutinin-neuraminidase (HN) and the fusion protein (F), V/phospho-/I proteins, matrix protein (M), large protein (L) and small hydrophobic proteins (SH). Currently, there are at least 12 genotypes composed by the sequence of the SH gene, where genotype G became the most frequently detected genotype in mumps outbreaks worldwide.
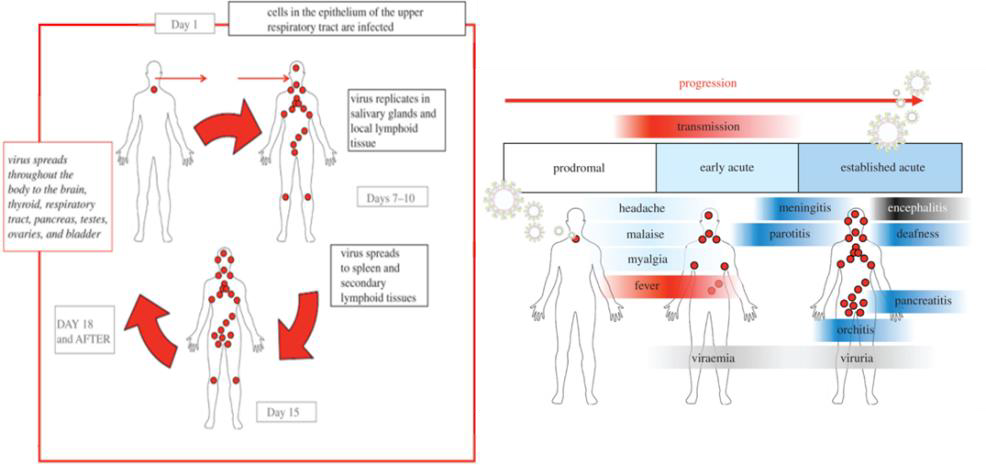
The mumps virus spreads through respiratory droplets when an infected person coughs, sneezes, or via direct contact with contaminated surfaces. Humans are the virus’s only natural host, as it binds to sialic acid receptors in the epithelial cells of the respiratory tract. The virus replicates and spreads systemically for 12–25 days before symptoms appear (incubation period). Approximately one-third of infected individuals experience sub-clinical infections with no symptoms, yet they can transmit the virus. Affected individuals may experience prodromal symptoms such as fever, myalgias, anorexia, malaise, headache, and nonspecific upper respiratory symptoms. The hallmark of mumps is inflammation of the salivary glands, leading to swelling of one or both parotid glands, accompanied by pain and discomfort in the cheeks and jaw area.
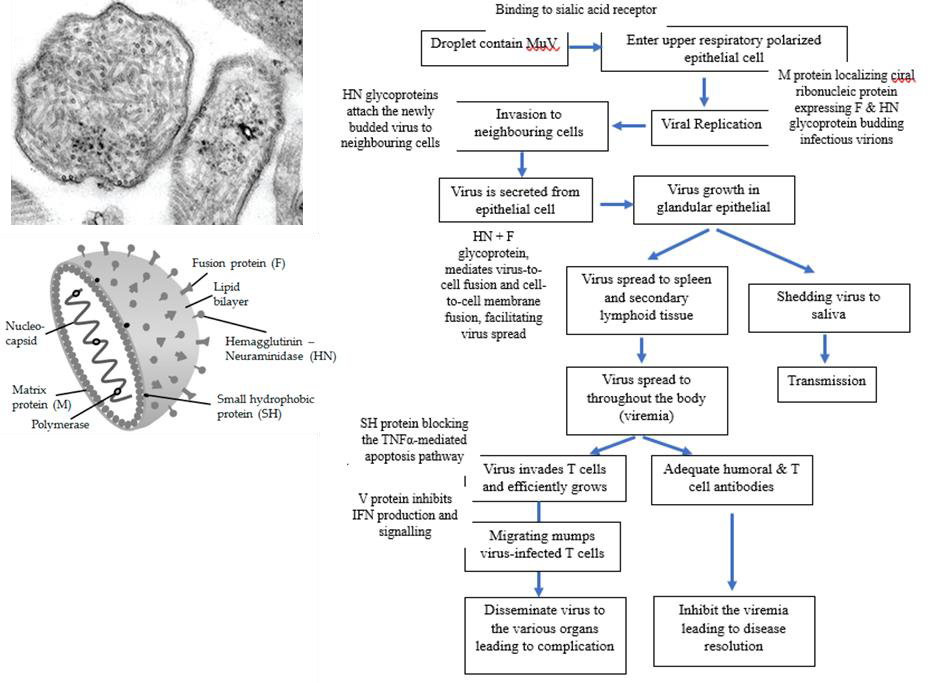
In complicated cases, mumps can result in meningitis, encephalitis, pancreatitis, hearing loss, oophoritis in females, or orchitis in males. The probability of developing orchitis is around 25% in post-pubertal males. Orchitis typically occurs 1–2 weeks after the onset of parotitis. Although mumps orchitis rarely results in sterility, it may contribute to subfertility. It can also lead to oligospermia, azoospermia, and asthenospermia (defects in sperm movement). Unilateral orchitis can significantly, though transiently, affect sperm count, motility, and morphology. Fertility impairment is estimated to occur in approximately 13% of patients with orchitis. However, 30%–87% of individuals with bilateral orchitis may experience infertility.
Clinical observation and laboratory testing are used to confirm a mumps infection. The preferred method of specimen collection is a buccal swab obtained within three days of parotitis onset, with laboratory confirmation achieved through rRT-PCR testing. Serology testing for IgM and IgG antibodies from paired serum samples may also aid diagnosis. However, the IgM response may not be detectable for up to five days after symptom onset in unvaccinated individuals and may be absent in vaccinated individuals. Mumps is typically a benign illness that resolves on its own within 10 days of symptom onset. Treatment primarily involves supportive care to alleviate symptoms. Patients with mumps should follow droplet precautions and remain isolated for 5–9 days after the onset of parotid swelling to reduce the risk of transmission.
Why does mumps keep coming back?
Despite the availability of effective vaccines, mumps outbreaks continue to be reported in various countries, raising the question: why does mumps keep coming back? To understand this, we need to explore several factors that may have contributed to the return of mumps.
Vaccine hesitancy and low vaccination rates
Although two doses of the MMR vaccine are claimed to be 88% effective against mumps, some individuals remain reluctant to get vaccinated. False claims about the MMR vaccine—particularly he unproven association between the vaccine and autism—have fueled widespread fear and mistrust. Despite extensive scientific studies disproving these claims, misinformation continues to circulate, influencing many parents to skip vaccinations for their children. The situation is exacerbated by the rise of anti-vaccine groups that actively oppose immunization and spread negative rhetoric about vaccines.
In countries where mumps has been nearly eradicated, a false sense of security may develop, with people perceiving the disease as no longer a threat. This perception can lead to complacency and lower vaccination rates. Additionally, the COVID-19 pandemic has disrupted vaccination programs globally, creating gaps in immunization coverage and leaving populations vulnerable to outbreaks.
In low- and middle-income countries, where mumps vaccination is not included in routine national immunization programs, low vaccination rates persist due to barriers such as limited awareness and financial constraints. Although the Pediatrician Association recommends the MMR vaccine in Indonesia, its uptake remains low. The government’s national immunization program only provides the MR (measles and rubella) vaccine for infants at nine months old, while the MMR vaccine must be sought privately. Many parents are reluctant to seek the MMR vaccine due to its cost and a lack of understanding about its importance. One mother interviewed stated that even if she could afford the vaccine, she did not see its value be-cause mumps is perceived as having low mortality.
Waning immunity and the need for booster doses
Over time, immunity to mumps can wane, leaving individuals who were previously infected or vaccinated at a young age more susceptible to the virus as they grow older. This is especially true for adolescents and young adults who received the vaccine in early childhood but did not receive a second dose. As these individuals enter their teenage and early adult years, they face a higher risk of contracting mumps and potentially spreading it to others. Research indicates that vaccine-derived immunity lasts an average of 27 years after the final dose is administered. This suggests that, in addition to the two doses typically given during childhood, a third dose at around age 18 may be necessary to maintain immunity into adulthood and reduce the risk of outbreaks.
Regarding concerns about certain mumps virus strains potentially escaping vaccine-induced immunity, a study was performed to address it. Sera from children collected six weeks after receiving the MMR vaccine were tested against selected group of genetically diverse mumps virus strains. While neutralizing antibody titers varied among strains, all were effectively neutralized, suggesting that immune escape is unlikely. Nonetheless, molecular surveillance and continued evaluation of vaccine efficacy remain crucial.
Population movement and crowded living conditions
With increasing global interconnectedness and easier travel access, the risk of mumps outbreaks is no longer confined to specific regions. Travelers with incomplete or no vaccination who visit en-demic or outbreak areas may contract the virus and potentially bring it back to their home. Mumps cases also tend to rise rapidly in crowded populations, where close contact significantly enhances viral transmission. Another contributing factor in such conditions is a lack of awareness. When mumps is perceived as a benign disease, this underestimation hinders prevention, early detection, and effective disease control efforts.
Lesson learned and the way forward
The resurgence of mumps highlights critical gaps in immunity, public awareness, and surveillance systems. A single case of mumps can lead to an outbreak in a community with low MMR vaccine coverage rates or with close contact. This poses a significant challenge for Indonesia as a developing, densely populated, tropical country with many infectious disease priorities. Educating the public is the top action for addressing this overlooked yet important viral infection. People need to understand that mumps is highly contagious and should practice health measures such as maintaining good hygiene (e.g., regular handwashing, using a mask, and proper cough/sneeze etiquette) and avoiding crowded places. Individuals should also seek appropriate medical consultation, avoid antibiotic misuse, maintain proper nutrition, and isolate if infected to prevent further transmission. Awareness of complications like orchitis, meningitis, or hearing loss is critical to timely medical intervention.
While we hope the government will include the MMR vaccine in the national routine immunization program, individuals who can afford it should be encouraged to get vaccinated. Promoting vaccination through partnerships with local leaders and health workers can help dispel myths about vaccine safety and improve vaccine acceptance within communities. With over 17,000 islands, Indonesia’s geography presents logistical challenges in delivering vaccines to remote areas. To address this, innovative solutions could include deploying mobile vaccination units and integrating vaccination drives into existing health outreach programs. Lastly, improving surveillance, notification, record keeping, and outbreak response systems is crucial for effectively controlling mumps. It’s time to designate mumps as a notifiable disease.
References
- Beleni AI & Borgmann S, 2018. Mumps in the vaccination age: global epidemiology and the situation in Germany. Int J Environ Res Public Health.
- Connell AR, et al., 2020. Mumps outbreaks in vaccinated populations—is it time to re-assess the clinical efficacy of vaccines? Front. Immunol.
- Di Pietrantonj C, et al., 2020. Vaccines for measles, mumps, rubella, and varicella in children. Cochrane Da-tabase Syst Rev.
- Kauffmann F, et al., 2021. Measles, mumps, rubella prevention: how can we do better? Expert Rev Vaccines.
- Lam E, Rosen JB, & Zucker JR, 2020. Mumps: an update o n o u t b r e a k s , v a c c i n e efficacy, and genomic diversity. Clin Microbiol Rev.
- Lau RK & Turner MD, 2019. Viral Mumps: increasing occurrences in the vaccinated population. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.
- Lewnard JA & Grad YH, 2018. Vaccine waning and mumps re-emergence in the United States. Sci Transl Med.
- Masarani M, Wazait H, & Dinneen M, 2006. Mumps orchitis. J R Soc Med.
- Principi N & Esposito S, 2018. Mumps outbreaks: a problem in need of solutions. J Infect.
- Rana MS, et al., 2023. The emergence of mumps after the COVID-19 pandemic in Pakistan: Time to consider MMR vaccination strategies. J Infect.
- Rubin S, et al., 2015. Molecular biology, pathogenesis and pathology of mumps virus. J Pathol.
- Rubin S, et al., 2012. Recent mumps outbreaks in vaccinated populations: no evidence of immune escape. J Virol.
- Su SB, Chang HL, & Chen AK, 2020. Current status of mumps virus infection: epidemiology, pathogenesis, and vaccine. Int J Environ Res Public Health.
- Tim Kerja Surveilans, Kemenkes RI. Webinar: meningkat-kan kewaspadaan pada mumps dan varicella. Available at: https://www.youtube.com/watch?v=LArT57AoIF4
- Dinkes DKI Jakarta. Sosialisasi kewaspadaan dini mumps (gondongan). Available at: https://www.youtube.com/watch?v=tNKGN6rEWUI&t=10152s
- https://www.antaranews.com/berita/4470097/kemenkes-kasus-gondongan-di-beberapa-daerah-masih-terkendali
- https://bblabkesmasmakassar.go.id/kenali-gejala-cara-penanganan-gondongan/
- https://www.pharmaceutical-technology.com/features/tracing-story-mumps-timeline/?cf-view

There is something unique about the management of mumps in Indonesia. A long-standing myth involves the use of “Blau,” a traditional blue powder used as an old-fashioned laundry bleach. It is believed that applying this powder to the swollen salivary glands can cure the disease. Some theories behind this myth suggest that the practice originated during colonial times as a way to mark individuals with mumps. Others believe that parents applied the powder intentionally to discourage children from touching the swollen area or to keep them embarrassed and confined at home. The practice has absolutely no curative value for mumps but may have been beneficial in isolating children and preventing the further spread of the virus
Leave a reply
Most Commented