Bridging The Gaps in Hepatitis B Vaccination in Indonesia:From Childhood Coverage to Adult Willingness
By: Cintya Naya Danastri, Ivana Yulian, Putri Permata Sari
What’s this about?
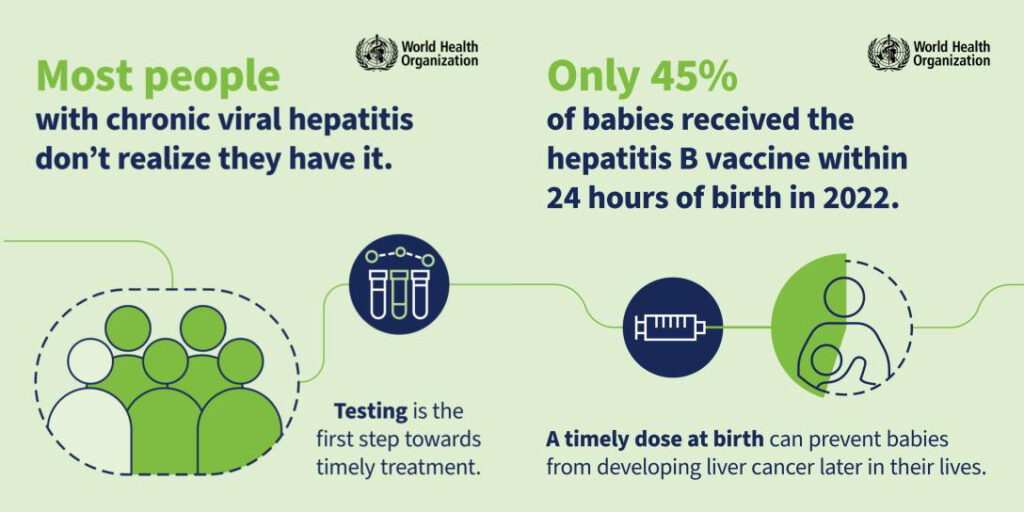
World Hepatitis Day, observed every year on July 28, is one of the World Health Organization’s (WHO) nine officially designated global public health days. It serves as a global call to action to raise awareness about the burden of viral hepatitis and to foster collective efforts toward its elimination by 2030. The theme for 2025, “Hepatitis: Let’s Break It Down”, highlights the urgent need to dismantle the financial, social, and systemic barriers that hinder prevention and care. It emphasizes simplifying, scaling up, and integrating hepatitis services, such as vaccination, safe injection practices, harm reduction, testing, and treatment, into national health systems. Among these, testing and treatment coverage remain critically low. Vaccination plays a crucial role in prevention, helping to reduce the burden on testing and treatment services.
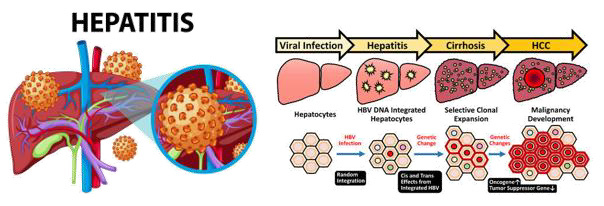
There are five main strains of the hepatitis virus – A, B, C, D, and E. Together, hepatitis B and C are the most common infections and result in 1.3 million deaths and 2.2 million new infections per year. Hepatitis B is a viral infection that causes inflammation of the liver and can lead to chronic disease, cirrhosis, or liver cancer if left untreated. Most people chronically infected with the Hepatitis B Virus (HBV) are unaware of their infection; thus, the disease often goes unnoticed and undiagnosed until the virus has caused severe liver damage. HBV is most commonly transmitted from mother to child at birth, but it can also spread through contact with infected blood or bodily fluids (e.g., saliva, semen, vaginal fluids).
How was the study conducted?
The first study used a large, nationally representative dataset from the 2017 Indonesia Demographic and Health Survey (IDHS). It employed a cross-sectional analysis of secondary data, focusing on mothers with children aged 1–3 years who had complete information on hepatitis B vaccination status. Mothers who were unaware of their child’s immunization history were excluded. The study examined the associations between potential factors and completion of the three-dose hepatitis B vaccine series using multivariable logistic regression analysis.
WHO Media Library
The second study also employed a cross-sectional design, conducted from February to March 2020, across 16 community health centers in Aceh and Yogyakarta provinces, which were selected for their contrasting hepatitis B vaccination coverage (highest in Yogyakarta and lowest in Aceh: 83.7% vs. 19.5% for complete vaccination, based on the 2018 national survey). Participants were outpatients or healthcare workers aged ≥15 years, physically healthy, willing to participate, and had not received hepatitis B vaccination as adults. Individuals with a history of HBV infection or prior vaccination were excluded. The survey collected data on sociodemographic characteristics, knowledge, attitudes, and willingness to receive the hepatitis B vaccine. Bivariate and multivariate analyses were used to identify factors influencing vaccine willingness.
What did the study find?
The first study analyzed data from 7,860 Indonesian mothers of children aged 12–59 months, revealing that about 10% of children were either never vaccinated or had received fewer than three doses of the hepatitis B vaccine. On average, children were 1.69 years old, with most living on Java (29.5%) and Sumatra (26.3%). Most parents had completed secondary education; 80% of fathers were employed, while more than 50% of mothers were housewives. Nearly half of the families belonged to the low-income group, and around 60% lacked health insurance. Most mothers reported using media regularly in the last year of the survey. Several parental and household factors were associated with higher odds of complete hepatitis B vaccination. Children of older mothers (≥30 years) had nearly twice the odds of complete vaccination than those of mothers aged 15-19 years. Secondary or higher parental education was linked to 2-fold higher odds of completion. Additional positive factors included regular maternal media exposure (AOR = 1.80), higher household income and health insurance coverage (AORs ≈ 1.5–1.6), and having two or fewer children (AOR = 1.90). Maternal employment (AOR = 1.20) was unexpectedly associated with complete vaccination despite known scheduling barriers, warranting further studies.
The second study surveyed 757 adults (373 from Aceh, 384 from Yogyakarta) at community health centers. About half of the participants in both provinces had previously heard about adult HBV vaccination, mainly through health providers and media (television and social media). However, participants in Yogyakarta had better knowledge of hepatitis B and its vaccine, greater risk perception, and higher willingness to be vaccinated (88% vs. 81% in Aceh). The most consistent predictor of willingness in both provinces was high risk perception, with higher odds in Yogyakarta (AOR = 5.11) than in Aceh (AOR = 2.58). In Yogyakarta, other positive predictors included female sex (AOR = 3.92), insurance coverage for vaccination (AOR = 4.80), and better HBV knowledge (AOR = 4.77). In Aceh, working in a high-risk healthcare setting was the only significant factor (AOR = 4.07). Religious concerns, especially doubts about the vaccine’s halal status, may partly explain lower willingness in Aceh, even among those with comparable knowledge. However, due to the small number of non-Muslim participants, the study cannot draw firm conclusions.
Why does this matter?
HBV remains a major global and national health threat. It contributes significantly to liver-related complications, including chronic hepatitis, cirrhosis, and hepatocellular carcinoma (HCC)—the sixth most common cancer and the fourth leading cause of cancer-related death. Although hepatitis B vaccination provides long-lasting protection for at least 20 years and has been included in the national childhood immunization program since 1997, coverage remains suboptimal. According to the 2018 National Health Survey, while 83.1% of infants received the timely birth dose, coverage for subsequent doses dropped to just above 60%. Although adult vaccination is recommended for high-risk groups, Indonesia has yet to implement a nationwide policy. A new regulation is being developed, starting with the voluntary immunization of healthcare workers.
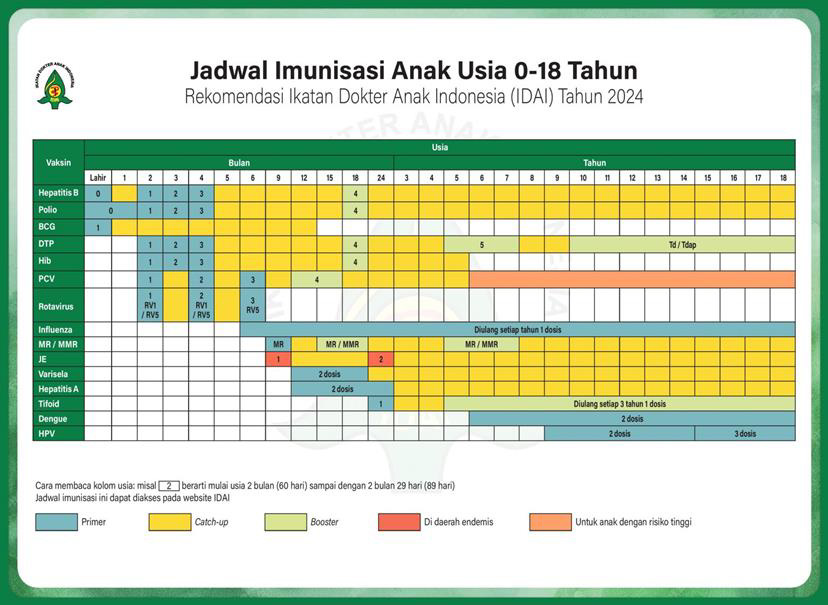
(https://www.idai.or.id/news news-event/agenda agenda-nasional/others/6798)
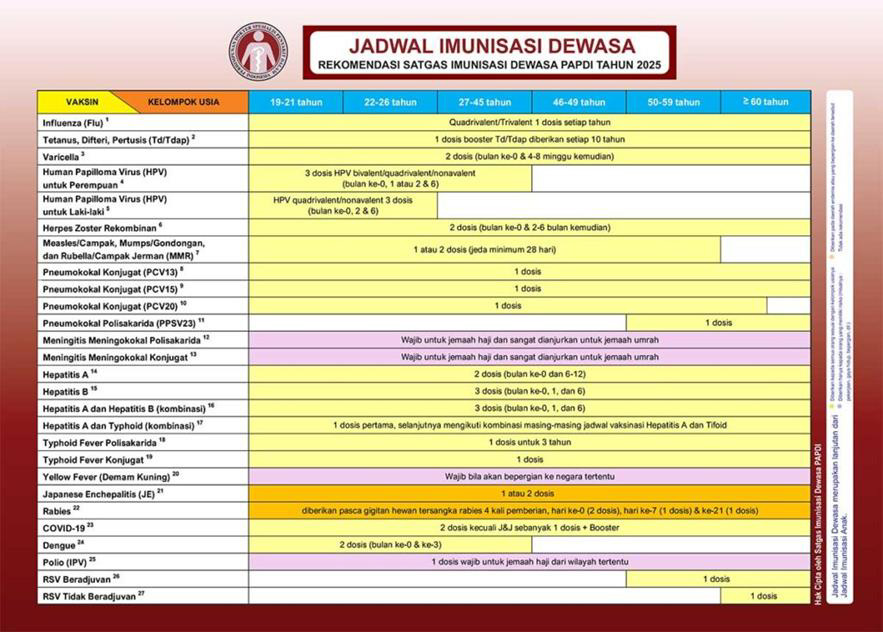
(https://satgasimunisasipapdi.com/jadwal jadwal-imunisasiimunisasi-dewasa/)
The two studies highlighted key barriers to HBV elimination through vaccination. The first revealed persistent socioeconomic disparities in childhood vaccination, even when vaccines are offered free of charge. Equitable healthcare access, reliable health information, and strategies to reduce economic and logistical barriers, especially in underserved communities, are critical to improving coverage. The second study found that perceived risk of HBV infection is the strongest driver of adult vaccination willingness in both Yogyakarta and Aceh. Regional and cultural contexts also shape acceptance. To increase adult hepatitis B vaccine uptake, efforts must include risk communication campaigns, expanded insurance coverage, and culturally tailored, locally relevant approaches. Strengthening both childhood and adult vaccination strategies is essential for Indonesia to meet its national and global hepatitis elimination goals.
Any limitations?
Both studies had notable limitations. The first study relied on secondary data, which had the potential for residual confounding due to the limited descriptions of key variables. For example, although some mothers were unemployed, the dataset did not capture whether they had sufficient free time to take their children for vaccination, creating the possibility of missed opportunities. Additionally, the study was unable to determine whether children were primarily cared for by their mothers or by other caregivers, particularly in households where mothers worked. This gap may have masked differences in vaccination uptake related to caregiving dynamics.
The second study faced potential selection bias, as most of the visitors in the included health centers were females, which may have limited the generalizability of the study’s results. Another limitation was that some studies had shown economic factors to be a significant factor in vaccination status (Chung et al., 2012; Park et al., 2012, 2013), but this was not included in this study due to the high amount of missing data. Additionally, with 95.9% of participants identifying as Muslims, the study could not fully explore religious influences on vaccine willingness. Lastly, social desirability bias may have influenced participants to provide favorable responses during interviews.
What’s next?
To support HBV elimination efforts, expanding public education on hepatitis is essential. Education should target various age groups and settings, including schools, workplaces, and community centers, with a focus on modes of transmission and prevention. Reiterating safe sex practices and personal hygiene guidelines can help reduce transmission risks. Primary healthcare facilities, being the most accessible to the public, have a vital role in both screening and early detection. While screening targets asymptomatic individuals at risk, early detection focuses on those presenting symptoms or with a family history of liver disease or autoimmune conditions. Strengthening both strategies can prevent disease progression and reduce long-term complications.
An important takeaway from the second study is the need for culturally sensitive, locally tailored strategies to improve hepatitis B vaccination uptake. Future research should investigate effective approaches to cultural and religious engagement that support vaccine acceptance. Expanding adult hepatitis B vaccine readiness assessments to other provinces would also provide a more representative picture of Indonesia’s diverse population and support nationwide planning efforts. Let’s break down the barriers—protect every liver, every life!
Article source:
Machmud P.B., Gayatri D, Astutik E. Complete dose of hepatitis B vaccination among children in Indonesia and factors associated: A community-based study. Kesmas. 2024 Aug;19(3):178-186.
Machmud P.B., Mikolajczyk R, Gottschick C. Understanding hepatitis B vaccination willingness in the adult population in Indonesia: A survey among outpatient and healthcare workers in community health centers. Jour-nal of Public Health. 2023 Dec;31(12):1969-1980.
References:
- Muljono, D. H. (2017). Epidemiology of hepatitis B and C in Republic of Indonesia. Euroasian Journal of Hepato-Gastroenterology, 7(1), 55. https://doi.org/10.5005/jp-journals-10018-1213
- Wang, S. H., Yeh, S. H., & Chen, P. J. (2021). Unique features of hepatitis B virus-related hepatocellular carcinoma in pathogenesis and clinical significance. Cancers, 13(10), 2454. https://doi.org/10.3390/cancers13102454
- Yano, Y., Utsumi, T., Lusida, M. I., & Hayashi, Y. (2015). Hepatitis B virus infection in Indonesia. World Journal of Gastroenterology, 21(38), 10714. https://doi.org/10.3748/wjg.v21.i38.10714
- World Health Organization. (2025). World Hepatitis Day 2025. Retrieved July 21, 2025, from https://www.who.int/campaigns/world-hepatitis-day/2025
- Ikatan Dokter Anak Indonesia. (n.d.). Agenda Nasional. Retrieved July 21, 2025, from https://www.idai.or.id/news-event/agenda-nasional/others/6798
- Satgas Imunisasi PAPDI. (n.d.). Jadwal Imunisasi Dewasa. Retrieved July 21, 2025, from https://satgasimunisasipapdi.com/jadwal-imunisasi-dewasa/
Most Commented