XENOTRANSPLANTATION: BELIEVE IT OR NOT?
Some of us may have heard the news about the first pig-to-human heart transplant that was conducted on 7 January 2022 in Baltimore, Maryland, USA. A new history has been made! However, this is not the first experience of transplanting animal organs to humans. Truth to be told, the attempt for do-ing xenotransplantation started many centuries ago. Before talking about the history and the steps leading to the success of this first pig-to-human heart transplant, let’s start with the definition. Again, this time, we will avoid discussing the ethical issues and public acceptance of such a procedure; let it be discussed on another day.
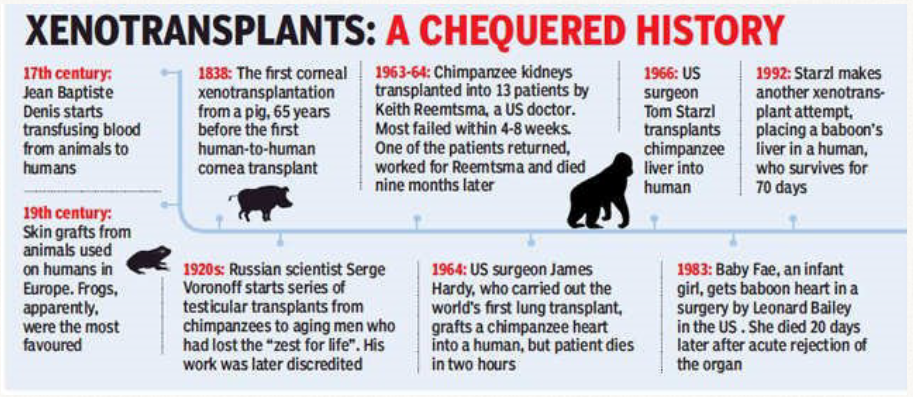
Based on Food and Drug Administration (FDA), xeno-transplantation is defined as any procedure that involves the transplantation, implantation, or infusion into a human recipient of either (a) live cells, tissues, or organs from a nonhuman animal source, or (b) human body fluids, cells, tissues, or organs that have had ex vivo contact with live nonhuman animal cells, tissues, or organs. Xenotransplantation has a long history going back to blood transfusions across species in the 17th century. Following the pioneering surgical work of Carrel, who developed the technique of blood vessel anastomosis, numerous at-tempts at nonhuman primate (NHP) organ transplantation in patients were carried out in the 20th century. In 1963–64, one patient returned to work for almost 9 months supported by a pair of chimpanzee kidneys. In 1964, the first (unsuccessful) heart transplant utilized a chimpanzee as the ‘donor’. A patient with a baboon liver transplant survived for 70 days in 1992. And many more….
However, there are several disadvantages with the use of NHPs as sources of organs and, with the advent of genetic engineering and cloning technologies, pigs are currently considered the animals most likely to resolve the problem of donor organ shortage. Some of the advantages: pigs have good breeding potential, short period to reproductive maturity (4-8 months), a decent number of offspring (5-12), adequate size of adult or-gans, significantly lower cost of maintenance, a distant relation of the immune system to human, considerable knowledge of tissue typing and experience with genetic engineering in pig, and low risk of transfer of infection.
The pathobiological barriers to successful pig organ transplantation in primates include activation of the innate and adaptive immune systems, coagulation dysregulation, and inflammation. The immunologic barriers to successful xenotransplantation are primarily related to the presence of natural anti-pig anti-bodies in humans and NHPs that bind to antigens expressed on the transplanted pig organ (the most important of which is galactose-α1,3-galactose [Gal]),5 and activate the complement cascade, which results in rapid destruction of the graft, a process known as hyperacute rejection.
Significant advances in recent years have been achieved with the advent of CRISPR–Cas9 genome editing, which made it easier to create pig organs that are less likely to be attacked by human immune systems. This first pig-to-human heart trans-plant used an organ from a pig with ten genetic modifications. The company that provided the pig heart knocked out three pig genes that trigger immune attacks and added six human genes that help the body to accept the organ. A final modification aims to prevent the heart from responding to growth hormones, ensuring that it remains human-sized.
Until today (11 February 2022), there is no bad news heard from the heart recipient. Let’s hope that he has a long and fruitful life. And let’s hope that xenotransplantation has a wonderful future as well.
References
- Pierson RN, Burdorf L, Madsen JC, Lewis GD, D’Alessandro DA. Pig‐to‐human heart transplantation: Who goes first? Am J Transplant. 2020 Oct;20(10):2669–74.
- McGregor CGA, Byrne GW. Porcine to Human Heart Transplan-tation: Is Clinical Application Now Appropriate? J Immunol Res. 2017:1–11.
- Deschamps J-Y, Roux FA, Sai P, Gouin E. History of xenotrans-plantation. Xenotransplantation. 2005 Mar;12(2):91–109.
- Cooper DKC, Gaston R, Eckhoff D, Ladowski J, Yamamoto T, Wang L, et al. Xenotransplantation—the current status and prospects. Br Med Bull. 2018 Mar 1;125(1):5–14.
- FDA. Xenotransplantation. 2021. https://www.fda.gov/vaccines-blood-biologics/xenotransplantation#
- Reardon S. First pig-to-human heart transplant: what can sci-entists learn? Nature News 14th January 2022. https://www.nature.com/articles/d41586-022-00111-9

all information here about liver are so informative and useful for everyone we also know website here about these information
Reply