ANTI-TUBERCULOSIS DRUGS RESISTANCE PATTERNS IN PULMONARY TB PATIENTS FROM SEVEN REFERRAL TB HOSPITALS: AN IMPERATIVE, DESCRIPTIVE PUBLICATION FROM THE INA-RESPOND TB STUDY
By: Nur Latifah Hanum & Adhella Menur
Before the COVID-19 pandemic, tuberculosis (TB) disease was the leading cause of death from a single infectious agent, Mycobacterium tuberculosis (MTB), ranking above HIV/AIDS. Almost one-third of the global population is infected with MTB, of which 1 in 10 will develop active TB, and the rest will define as latent TB. This high proportion of latent infections implies long co-evolution between MTB and its human hosts. The latency can last for decades, only flaring into active disease when the person is weakened by hunger, old age, or other immunocompromised states. Even though Robert Koch first introduced MTB on March 24, 1882, genetic analyses of this airborne bacteria worldwide suggest that it evolved tens of thousands of years ago. An astonishing discovery in 2008 confirmed the theory, which revealed a successful MTB DNA extraction from the bones of a mother and baby buried 9000 years ago, found at Atlit-Yam, Israel, a prehistoric village that now lies beneath the waters of the Mediterranean Sea. That made us wonder, decades after decades with numerous scientific breakthroughs, why can’t we combat this curable ancient pathogen? (1, 2)
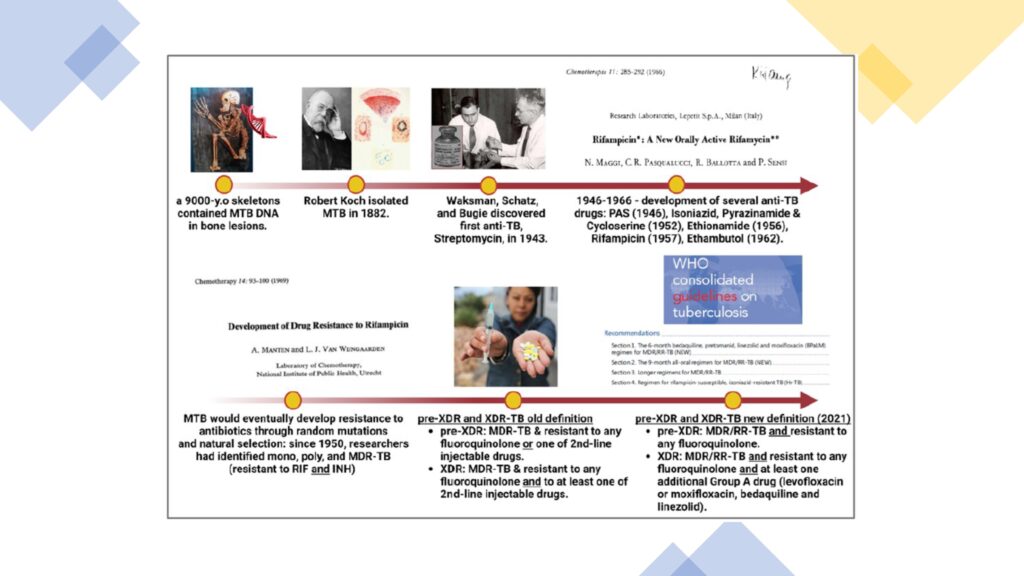
MTB has unique biological features, such as a thick and lipid-rich cell envelope, very slow asymmetrical division, and antibiotic-degrading and modifying enzymes that lead to anti-TB drug resistance. The general hypothesis that resistance always conferred a loss of bacterial fitness and hence led to lower case fatality rates and decreased transmission had been disputed by MTB. Since the first anti-TB drug discovery, Streptomycin, in 1943 and followed by other drugs, resistance always has escorted it. The incidence of drug-resistant (DR) TB has increased yearly and continues to be a public health threat due to high morbidity, mortality, and devastating socioeconomic impacts. Rifampicin (RIF) resistance (RR) – the most effective first-line drug – is of greatest concern. Resistance to RIF and isoniazid (INH) is defined as multidrug-resistant TB (MDR-TB). MDR/RR-TB requires treatment with second-line drugs, which are long and disturbing. In 2021, there were an estimated 450,000 incident of MDR/RR-TB cases worldwide; 3.6% among new cases and 18% among those previously treated. Indonesia is listed as the second highest TB burden country in the world and amongst the seven countries that accounted for two-thirds of global MDR/RR -TB cases. Worryingly, only 35% of 24,000 estimated MDR/RR-TB cases were laboratory confirmed, of which 60% of patients were initiating treatment, and <50% were successfully treated (1, 3, 5-7).
In 2017-2020, INA-RESPOND conducted a prospective cohort study of adult pulmonary TB patients at seven DR-TB referral hospitals in seven large cities in Indonesia (Dr. Soetomo, Surabaya; Sanglah, Denpasar; Dr. Sardjito, Yogyakarta; Dr. Kariadi, Semarang; Persahabatan, Jakarta; H. Adam Malik, Medan; and Dr. Wahidin Sudirohusodo, Ma-kassar) namely TRIPOD (Tuberculosis Research of INA-RESPOND On Drug Resistance, NCT02758236) study, with dr. Erlina Burhan, Sp.P(K) as the national principal investi-gator. At that time, Indonesia’s anti-TB drugs resistance testing rates are lower than global testing rates and there was lacking data for DR-TB, particularly amongst newly diagnosed TB cases. The TRIPOD primary objective was to estimate the proportion of MDR-TB amongst newly diag-nosed and previously treated pulmonary TB cases. During study baseline period, before 7 days of anti-TB treatment, sputa from participants were collected to be tested for acid-fast bacilli (AFB) smear, Xpert MTB/RIF, MTB culture, and drug susceptibility test (DST) at appointed National TB Program (NTP) reference laboratories. Among those with positive MTB culture and had DST results, participants were further categorized as having drug-sensitive/susceptible TB (DS-TB), mono-resistance TB, poly-resistance TB, MDR-TB, pre-extensively (pre-XDR-TB), and XDR-TB based on updated WHO 2021 criteria. Two years after the study ended, the first manuscript of the TRI-POD study was published on October 17, 2022, in the American Society of Tropical Medicine and Hygiene journal, entitled “Characteristics of drug-sensitive and drug-resistant tuberculosis cases among adults at tuberculosis referral hospitals in Indonesia” doi: 10.4269/ajtmh.22-0142.
Among 447 participants with complete AFB, GeneXpert MTB/RIF, and sputum culture results, 260 (58.2%) were classified as newly diagnosed TB and 187 (41.8%) as previously treated TB cases. Sputum culture was positive in 173 (66.5%) newly diagnosed TB and in 139 (74.3%) previously treated TB cases. Based on DST results of 312 participants, 158 (50.6%) were still classified as DS-TB; 66.5% (115/173) in newly diagnosed TB and 30.9% (43/139) in previously treated TB cases. Mono resistance was more frequent in newly diagnosed TB versus previously treated TB cases (32.8% versus 14.6%). MTB resistant to either RIF or INH dominated the mono- and poly-resistant sub-groups for both newly diagnosed TB (73.7% and 61.5%) and previously treated TB (64.3% and 88.9%) cases. The proportion of MDR and pre-XDR was 46% (64/139) and 6.5% (9/139) in previously treated TB and 13.3% (23/173) and 1.7% (3/173) in newly diagnosed TB cases. Only one of the newly diagnosed DR-TB cases had prior contact with DR-TB patients. Thus, most of newly diagnosed DR-TB cases did not have a clearly identifiable source of resistance. Cavities in the chest X-ray and diabetes mellitus were common in DR-TB participants (8).

In the TRIPOD study, the proportion of MDR-TB among newly diagnosed TB and previously treated TB cases was much higher than reported in the WHO Global TB Report.
This large discrepancy may be attributable to lack of recent TB surveillance in Indonesia, which was last conducted in 2013–2014. Additionally, TRIPOD participants were recruited from referral hospitals, whereas previous surveys recruited from community health centers. Most participants had sought treatment both in public and private facilities before being sent to the referral hospitals, suggesting the population represented more difficult cases. Further characterization of Indonesia’s TB epidemiology in the general population is needed (8).
Identification of 58 (33.5%) participants with DR (32 mono/poly-resistant, 23 MDR, and three pre-XDR) among those without previous exposure to anti-TB drugs supports reports that primary DR-TB has increased up to 80% in some settings. However, the study cannot exclude the possibility that patients were incorrectly categorized as treatment-naive because prior anti-TB drug use may not have been accurately reported. The high incidence of DS- and DR-TB cases in previously treated individuals underlines the high risk of recurrent TB in this population and contributes substantially to disease burden. Post-treatment follow-up that anticipates TB relapse and secondary preventive therapy may accelerate reduction of TB incidence and save resources for TB control (8, 9).
Mandatory DST to first-line drugs in the TRIPOD study enabled detection of a high proportion of MTB isolates resistant to INH in non-MDR/XDR groups (22 of 213 patients (10.3%)). Access to DST remains low particularly for newly diagnosed TB patients, consequently INH resistance is often undetected in daily practice because the more readily available rapid diagnostic test (Xpert MTB/RIF) detects only RR. If INH resistance is not seen, patients will receive drugs for DS-TB, which is suboptimal for DR-TB and increases the risk of treatment failure, relapse, or acquiring RR. In the TRIPOD study, among 167 patients with RIF sensitive by Xpert, 15 (9%) were INH resistant by DST. A recent large whole genome sequencing (WGS) study revealed that INH resistance may predate RR. In the current WHO guidelines for DR-TB treatment, patients with confirmed RIF-susceptible, INH-resistant TB (Hr-TB) are recommended to be treated with rifampicin, ethambutol, pyrazinamide, and levofloxacin for six months (4, 8).
This manuscript highlights the need to improve current public health approaches to TB in Indonesia. Because primary DR-TB was relatively high, community transmission must be addressed by screening programs and tracking of case contacts followed by more liberal use of DST, for which Indonesia has low uptake. Comprehensive drug-resistant data will allow patients to be treated with effective drugs, reduce development of drug resistance and toxicity, and inform public health program treatment algorithms. Early detection and adequate treatment will reduce transmission, morbidity, and mortality. In addition, strengthening public–private partnerships and improving coordination between the national health insurance scheme and the NTP will reduce diagnostic delays and minimize costs.
The TRIPOD findings offered crucial data to the TB community on the serious threat of DR-TB transmission in Indonesia. The threat is worsening after the damaging impact on access to TB diagnosis and treatment during the COVID-19 pandemic. Notwithstanding, there are silver linings in every circumstance. The COVID-19 pandemic increases government and public awareness regarding the importance of pathogen surveillance, health protocols, transmission control, and healthcare equity. It also accelerates the deployment of rapid molecular testing, WGS, and resources training. In 2022, the country owned 21 national TB laboratories qualified for MTB culture; 12 can perform DST for rifampicin, isoniazid, moxifloxacin, levofloxacin, amikacin, bedaquilin, linezolid, clofazimine, and pyrazinamide, and seven can perform line probe assay (LPA). 1819 Xpert MTB/RIF available in 34 provinces, with a plan to expand Xpert MDR/XDR, which provides rapid detection of isoniazid, fluoroquinolones, and second-line injectables resistances (7). Eighteen sequencer ma-chines, as a part of the COVID-19 response mechanism, will distribute to enhance genomic surveillance and drug resistance for various pathogens, including MTB (10).
Finally, we need to embrace a powerful message of the opening remark from the WHO director in the global TB report 2022. Quoted, “If the COVID-19 pandemic has taught us anything, it’s that with solidarity, determination, innovation and the equitable use of tools, we can overcome severe health threats. Let’s apply those lessons to TB. It is time to put a stop to this long-time killer. Working together, we can end TB.“(1)
More to read
- WHO. Global tuberculosis report 2022. 2022.
- Levy S. The evolution of tuberculosis: genetic analysis of-fers new insight on the spread of an ancient disease. Bio-Science. 2012.
- Keshavjee S, Farmer PE. Tuberculosis, drug resistance, and the history of modern medicine. N Engl J Med. 2012;367(10):931-6.
- WHO. WHO consolidated guidelines on tuberculosis. Mod-ule 4: treatment – drug-resistant tuberculosis treatment. 2022.
- Gygli SM, Borrell S, Trauner A, Gagneux S. Antimicrobial resistance in Mycobacterium tuberculosis: mechanistic and evolutionary perspectives. FEMS Microbiol Rev. 2017;41(3):354-73.
- Aldridge BB, Fernandez-Suarez M, Heller D, et al. Asym-metry and aging of mycobacterial cells lead to variable growth and antibiotic susceptibility. Science. 2012;335(6064):100-4.
- Indonesia MoH. Dashboard TB Indonesia 2022 [Available from: https://tbindonesia.or.id/pustaka-tbc/dashboard-tb/].
- Burhan E, Karyana M, Karuniawati A, Kusmiati T, Wibisono BH, Handayani D, et al. Characteristics of Drug-sensitive and Drug-resistant Tuberculosis Cases among Adults at Tuberculosis Referral Hospitals in Indonesia. Am J Trop Med Hyg. 2022.
- Cox HS, McDermid C, Azevedo V, Muller O, Coetzee D, Simpson J, et al. Epidemic levels of drug resistant tubercu-losis (MDR and XDR-TB) in a high HIV prevalence setting in Khayelitsha, South Africa. PLoS One. 2010;5(11):e13901.
- Dirjen P2P kunjungi laboratorium FK UNDIP sebagai salah satu calon laboratorium penempatan mesin WGS 2022 [Available from: http://p2p.kemkes.go.id/7687-2/].

Most Commented